Bursting the Coronavirus Hype Bubble
Overview
The phrase "coronavirus hype bubble" refers to misinformation and hyperbole about the novel coronavirus. The virus is not a hoax, but it's not anywhere nearly as bad as you've been led to believe. It is mild for most, but it can cause serious disease in a miniscule portion of people, particularly the elderly.
Early in the Spring, it seemed that some of the response to the new SARS-CoV-2 coronavirus was not based on evidence. And I think many of us in the technology world thought the same thing.
When you work in IT for a long time, you develop a sixth sense for when things just don't add up. Having to make decisions based on data—and then being held responsible for those decisions—tends to sharpen one's critical thinking skills. More to the point, IT work entails technology, engineering, and math, and these are the same skills required to analyze and understand the data regarding the novel coronavirus.
Getting the right data
One thing you learn from troubleshooting is that you need the right data. When a user is dealing with a problem, they may offer a lot of facts that may or may not be relevant to the issue at hand. As an IT professional, your job is to determine what data is relevant. When it comes to the virus, there are only two metrics that matter:
- The percent of positive tests—the number of positive tests divided by the number of total tests.
- The number of deaths caused by infection
The percent of positive tests
The percent of positive tests metric is more important than the absolute number of cases because the number of cases depends on the number of tests. All things being equal, if you do more tests, you show more cases. If you do fewer tests, you show fewer cases. In statistical terms, the number of tests is a counfounding variable because it influences the number of cases in an unpredictable way.
Until testing became widespread, we didn't have a good grasp of the percent of people infected. We were testing only people with severe symptoms, which led to the false impression that percent positives were higher than they were. When extrapolating these inflated numbers to the whole population, it led to some silly and irresponsible predictions that we now know are wrong.
The number of deaths
The number of deaths is significant because it gives us an idea of just how bad the virus is, and that should inform how we deal with it. Two things became became clear early on.
One. For children, the risk of the virus causing serious illness is virtually zero. According to Dr. Scott Atlas of the U.S. coronavirus task force:
Children are a very low-risk population. There is virtually zero risk of death and low risk of hospitalization.
Two. The virus can cause serious and life-threatening illness in the elderly and people with compromised respiratory, immune, or vascular function. But if you're healthy and under 60, your risk is extremely low.
Most people may never get sick
In the U.S., events were cancelled and businesses were closed for months. Almost everyone has made the assumption that the virus could spread through the entire population. But the data suggests that only about 20% of the population is susceptible to significant illness from the coronavirus. According to a German study, 81% of people who have never been exposed to the coronavirus show T-cell activity against it:
Cross-reactive SARS-CoV-2 T-cell epitopes revealed preexisting T-cell responses in 81% of unexposed individuals, and validation of similarity to common cold human coronaviruses provided a functional basis for postulated heterologous immunity
In other words, if the other coronaviruses that cause the common cold confer some immunity to SARS-CoV-2, then most of the population may not get sick from the virus at all, or if they do, will have only a mild case.
Herd immunity works
Herd immunity is the phenomenon that when a certain percentage of the population develops immunity to a virus, it protects the rest of the population that doesn't have immunity. The percent of the population that has to be immune to a virus for herd immunity to kick in varies by virus, but it's typically between 80%-95%.
In March, the Diamond Princess cruise ship had an outbreak, and only 19.2% of the occupants tested positive. Cruise ships are notorious for being incubators for outbreaks, so the Diamond Princess was an ideal petri dish for the virus. But despite this, 80% of the occupants did not get infected. Another ship, the Grand Princess, also had an outbreak and its occupants had a percent positive rate of only 16.6%. Are you seeing a pattern? The innate immunity always seems to be around 80%.
Once 16%-20% of people get infected, the virus seems to hit a wall. This is based on two small sample sizes, but if we take much larger samples from states and even countries, we see that it pans out.
Of everyone who has been tested for the coronavirus in the U.S., 18% have tested positive. If past experience is any indicator, we are close to reaching herd immunity, if we haven't reached it already.
Sweden was right: Shutdowns didn't work
Now here's something that's going to blow your mind. There's one country that didn't shut down at all: Sweden. Sweden never shut down, and they got to herd immunity within a few months. In the following chart, look at how Sweden's curve begins to flatten in late July, marking the point at which they began to hit herd immunity. Compare this with the U.S. where the number was still sharply increasing.
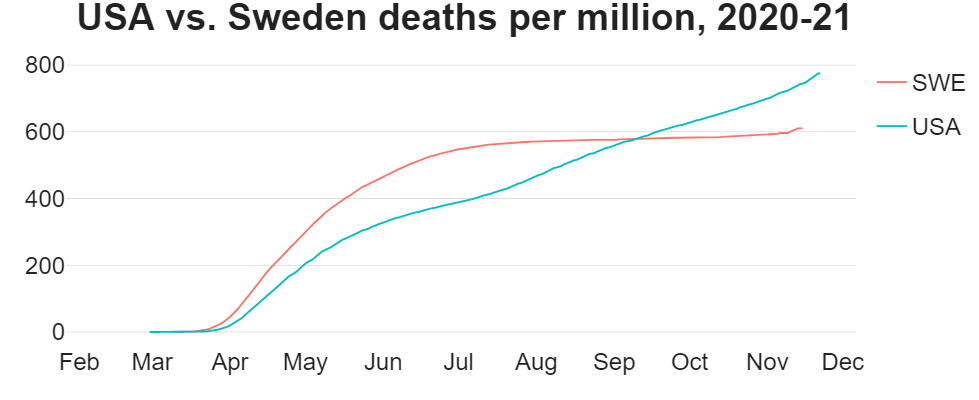
Proportionally to population, Sweden has had fewer deaths than the U.S. As of this post Sweden has 819 deaths per million, and the U.S. has 1044. But as you can see, the U.S. curve hasn't even begun to flatten. Shutdowns that were designed to "flatten the curve" didn't work, and the curve kept growing.
Now let's look at the percent of positive tests shown in the following chart. Notice that during the time the U.S. was shutdown, Sweden's percent positives stayed up because they allowed the virus to burn through the population. Then at the beginning of July, Sweden's percent positive rate dropped precipitously and remained low, which matches the flattening of the deaths-per-million curve.
The percent positives remained low until November, which is when the weather there begins to get cold. Cold weather always brings an increase in respiratory illnesses, and this virus is no different. Both Sweden and the U.S. are going to see weather-related spikes in illness, and this is to be expected.
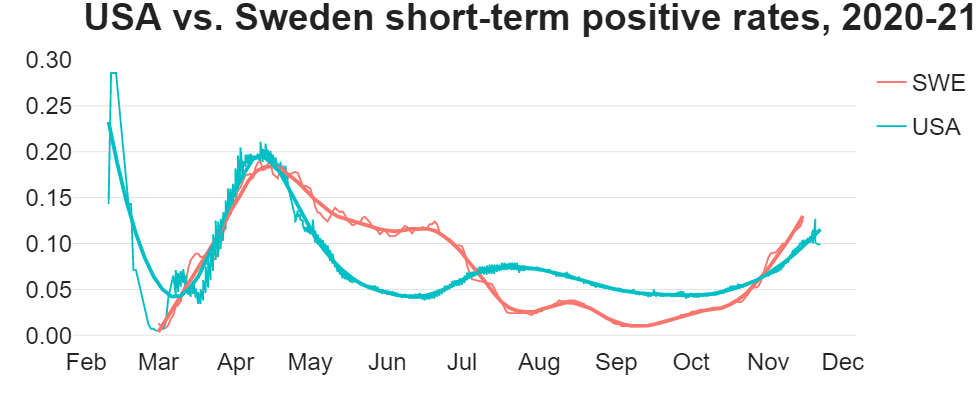
The U.S. saw a drop in April and May because everything was shut down. But starting in late June, we saw an increase that coincides with the reopenings. The virus arrived in both the U.S. and Sweden at almost exactly the same time and peaked at the same time, but Sweden began to hit herd immunity faster.
Immunity can wane over the course of months or—more commonly—years. This is why you have to get boosters for certain vaccines. It's likely that SARS-CoV-2 is going to be endemic, meaning it's not going away. Most people will develop immunity to it, either through being exposed to it or getting vaccinated, but some people will not develop immunity. The bottom line is that we should expect the virus to remain with us indefinitely.
There's a myth that once you get sick from the virus, you can get sick from it again and again. This is false. Once you get sick and recover, you develop antibodies that protect you in the short term (a few months). You also develop memory B-cells and memory T-cells that protect you over the long term (years).
Note: I created these graphs using the R programming language. You can download the code as a Jupyter notebook to recreate the graphs yourself.
The total death count is unknown
The actual number of deaths from the virus (and not just with it) is unknown. What we do know is that the CDC guidance allows a death to be counted as a coronavirus death even with a negative test. A positive test is not required to code a death as a coronavirus death. Furthermore, if someone tests positive and dies, that death may still be counted as a coronavirus-related death, regardless of the surrounding circumstances. That means, for example, if someone gets seriously injured in a car accident then later dies, they may be counted among the SARS-CoV-2 deaths as long as they test positive. If there's any doubt whether the coronavirus contributed to a death, doctors generally err on the side of assuming it was.
The guidelines are to streamline recordkeeping because conclusively determining a cause of death takes time. The CDC is more concerned with gathering statistics rapidly, even if they're not 100% accurate. This is just common sense. Anyone who attributes this process to malice has watched too many movies. Likewise, anyone who says that this is a conspiracy theory is promoting ignorance and denialism of the CDC's own guidelines and data.
Deaths not undercounted
Some have claimed—without evidence—that deaths might be undercounted. Very early on when testing wasn't widely available and not everyone was looking for the virus, this was a reasonable concern. But today it's virtually impossible that a death caused by the virus will be missed. Everyone is looking for cases, and testing is widespread. If there's even a hint that a death is related to the virus, the person will be tested. Depending on the circumstances, they may be counted as a coronavirus death even without a positive test.
You might wonder, if the death count is unknown, how do we know that the deaths per million is accurate? I think the actual U.S. deaths count may be a bit lower, because if it is accurate, then the U.S. is going to end up with a disturbingly high number by the time we're done. However, regardless of how accurate the number is, the fact remains that the U.S. shutdowns did not flatten the curve. Sweden's herd immunity strategy did.
The CDC's estimated death rate
The CDC estimates that the death rate for the virus is about 0.065%. However, the current death count stands at about 180,000, and there are almost 6 million cases. That yields an overall death rate of 3%. Why is there such a discrepancy between the CDC's estimate and the calculated rate? The CDC's answer:
we have replaced the Symptomatic Case Fatality Ratio and the Symptomatic Case Hospitalization Ratio with the Infection Fatality Ratio (IFR), which takes into account both symptomatic and asymptomatic cases and may therefore be a more directly measurable parameter for disease severity.
Essentially, the CDC seems to be assuming that the real number of cases is 4.5 times higher than what's reported. Right now, there are about 6 million reported cases, so the actual number of cases would be 25 million. 25 million people happens to be about 8% of the U.S. population, a number that jives perfectly with the current total percent positive rate.
It's worth noting that what the CDC calls "asymptomatic" spread likely refers to people with mild symptoms. True asymptomatic spread—that is, spread by people who have the virus and have zero symptoms—almost never happens.
Epidemiological models were doomed from the beginning
By now, everyone knows that the predictions by the Institute for Health Metrics and Evaluation (IHME) and the Imperial College London were wrong. But why were they wrong? The answer is so simple that it might even make you angry.
All the epidemiological models assumed that everyone was susceptible to infection!
As we've established based on the percentage of positive tests, most people may never get infected. But the models assumed everyone will eventually get infected. To truly appreciate why this is such a wrong assumption, let's look at a classic epidemiological model.
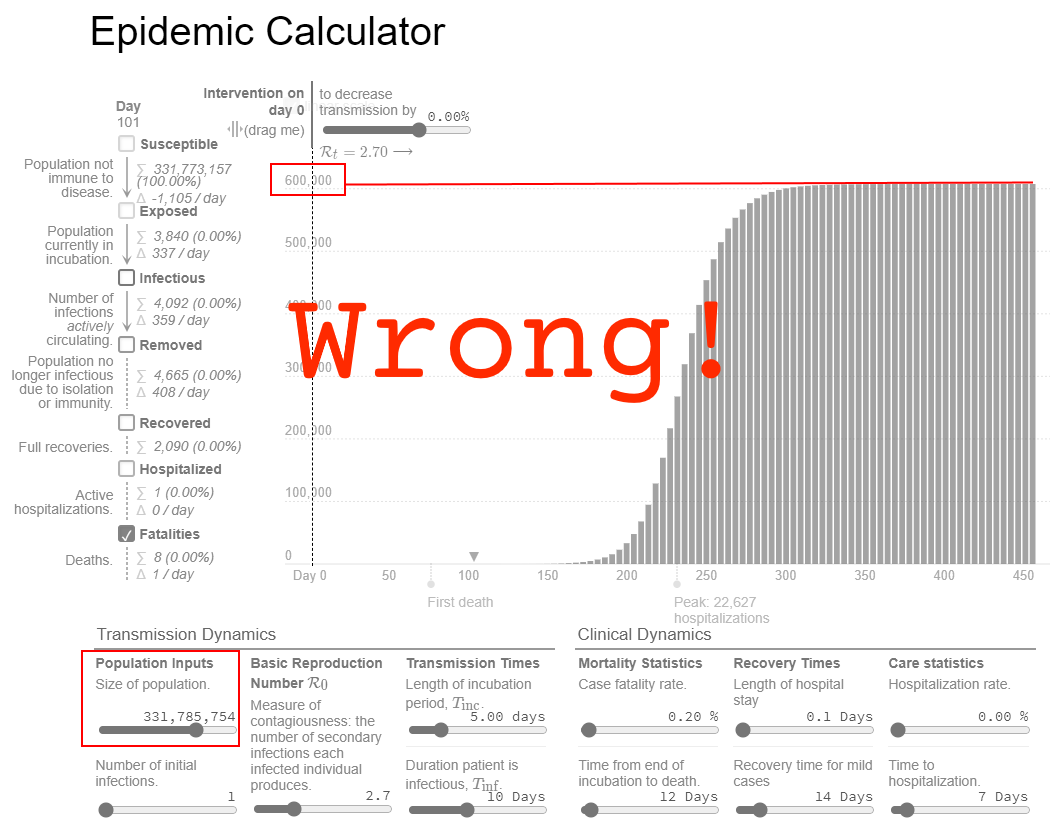
I plugged the CDC's numbers into a model that assumes a population of about 330 million people (the population of the U.S.), and the results just didn't seem believable. This ridiculous result shows over 600,000 deaths! But deaths peaked months ago, and the current count is about 180,000. There's no way we'll ever get anywhere close to 600,000 deaths.
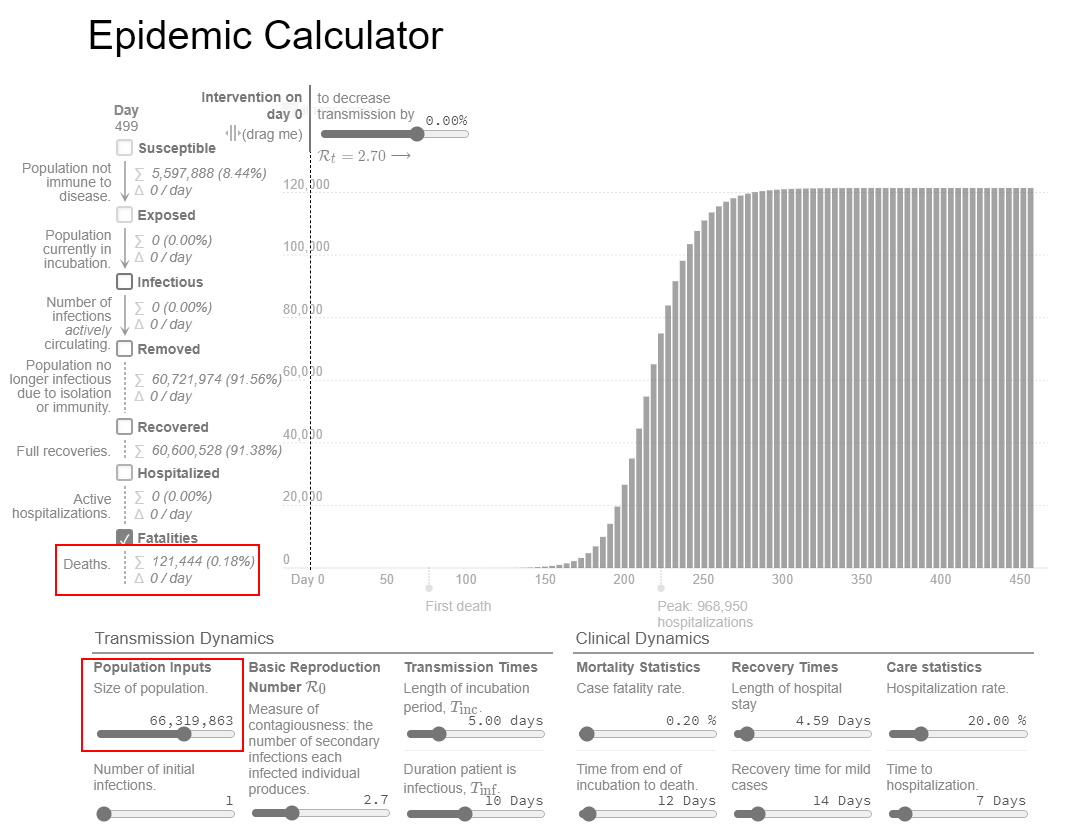
Now let's try different numbers. If we assume that only 20% of the population (66 million people) could even get seriously sick from the virus, the model looks dramatically different. It shows a total of about 120,000 deaths, which is much closer to the current count.
Masks don't work
Masks just don't work. It would be nice if they did, but they don't. The data all but proves it. A study published in the Annals of Internal Medicine concluded that general mask usage doesn't reduce community spread:
...a recommendation to wear a surgical mask when outside the home among others did not reduce, at conventional levels of statistical significance, incident SARS-CoV-2 infection compared with no mask recommendation...
Dr. Scott Atlas stated it succinctly when he said: "Masks work? NO"
The CDC even tacitly admits the ineffectiveness of masks. When it comes to people with exposure or potential exposure to an infected person, the CDC recommends quarantining for 14 days...
... irrespective of whether the person with COVID-19 or the contact was wearing a mask or whether the contact was wearing respiratory personal protective equipment (PPE)
The CDC is careful to say only that masks may work because they know there's no scientific evidence that they do. Whatever effect masks might have is minimal. The Norweigan Institute of Public Health had this to say about it:
Assuming that 20% of people infectious with SARS-CoV-2 do not have symptoms, and assuming a risk reduction of 40% for wearing facemask, 200 000 people would need to wear facemasks to prevent one new infection per week in the current epidemiological situation.
Assuming a 40% reduction flies in the face of evidence, as the Danish study suggests the reduction is somewhere around 2%—statistically insignificant.
If you know anyone who is at high risk, make sure they understand that masks are unproven. They may choose to wear one regardless, but they should take precautions as if they're not wearing one at all.
If masks were effective, you would expect that areas where mask-wearing is common to have a lower percent of positive tests. But that's not what we see. Instead, in some cities that enacted mask requirements, the number of cases went up. But in other cities, cases went down. Obviously, masks had nothing to do with the number of cases changing. Rather, it's all about the timing. Places that required masks early saw the cases go up. Places that waited until later saw cases drop because the virus had already peaked on its own.
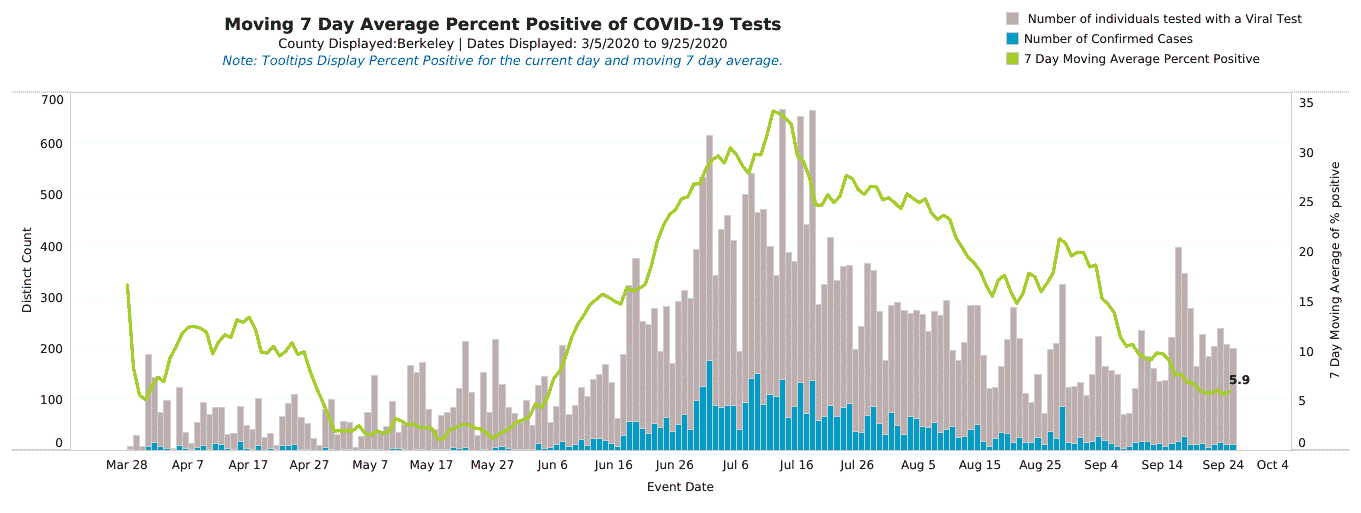
To really appreciate the insignificance of mask wearing, it's instructive to compare two counties side-by-side. In South Carolina, Charleston county has had a mask ordinance since late June.
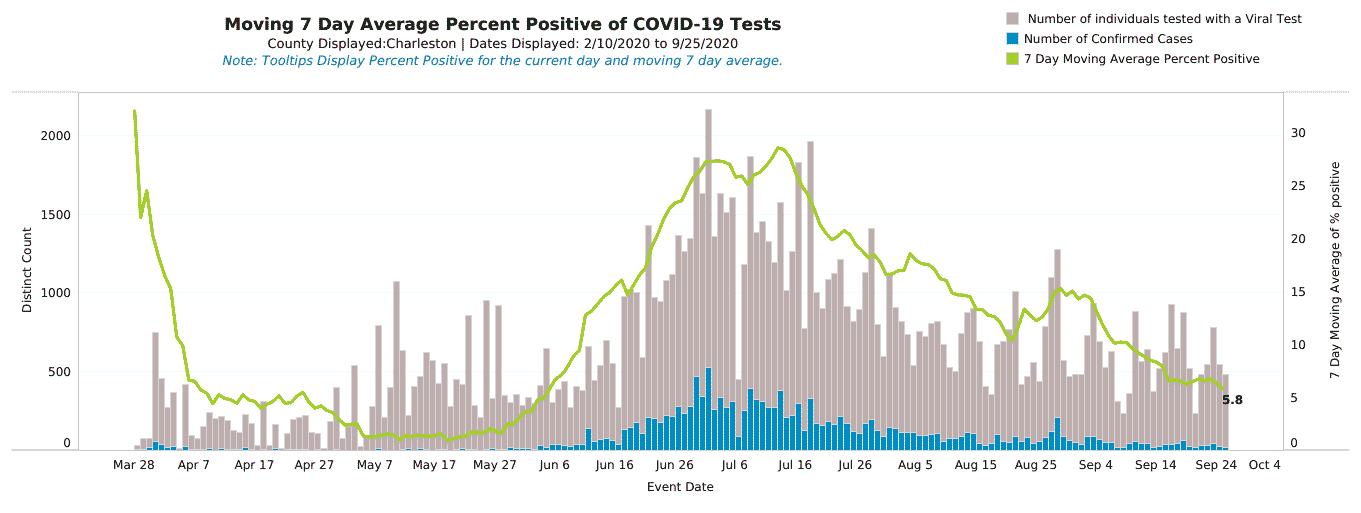
Neighboring Berkeley county, on the other hand, has never had a mask ordinance. Notice how the peaks and valleys occur in the same places and the overall percent positive follows the same trajectory in both counties.
Masks don't move the needle
In other places, masks seem to make no difference one way or another. For example, on July 16, Colorado enacted a statewide mask mandate, and the percent of positive tests was at 7%. Three weeks later, the percentage was still at 7%. On August 15, the percent of positive tests was still 7%. Masks literally made zero difference.
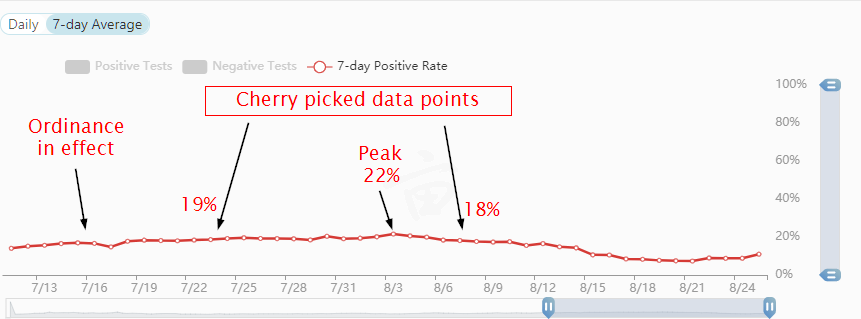
Another example is Alabama. When their mask mandate began on July 16, percent positives were at 17%. About two weeks later, on August 3, that number peaked at 22%. As of August 31, percent positives are still at 17%. Masks didn't work.
Hawaii has been under a mask mandate since April 2020. On August 26, they saw the percent of positive cases peak at 11%. Masks didn't work.
Regardless of where you look, the percent of positive cases always tops out around 22%-24%. One could argue that without masks, Alabama's peak would have been higher. However, the Diamond Princess and Grand Princess cases weigh heavily against that possibility. They weren't wearing masks, and the percent of positive cases didn't exceed 20%.
Percent of positive tests increased after mask requirements
In many places that have been requiring masks for months, the percent of positive tests is increasing! People who were quick to tout the benefits of masks are now eating their words as the percent of positive tests is increasing in areas that have had mask mandates for weeks if not months.
In late June and early July, some of the largest cities in South Carolina enacted mask ordinances. Columbia and Greenville saw cases increase, whereas Charleston saw them go down. Those in the latter group patted themselves on the back, believing that masks were to credit. Well, now South Carolina is seeing a significant spike in the percent of positive tests, between 21%-24%. Masks didn't work.
The Masks & COVID-19 interactive tool lets you look at the correlation between mask wearing and cases or deaths at the state and county level.
Unfortunately, some media outlets have cherry-picked data that shows cases going down after mask rules went into effect, perpetuating the unproven claim that masks are effective against the virus. This is the sort of confirmation bias that has always fueled junk science claims, like cell phones causing cancer. You can easily spot such sloppy stories by the fact that they focus on the absolute number of cases instead of the percent of positive tests. This Newsweek article on Alabama's mask mandate is one such example:
[T]he state's average daily case count has been on a downward trend from late July, just days after a statewide mask mandate was issued on July 15. After peaking on July 24, the state's three-day moving average of new cases mostly decreased to August 5...
Where the article does make mention of the state's percent positives, it again cherry picks two data points that paint a false picture:
The average percentage of positive tests in Alabama reported over the past week was 18.1 percent, a slight drop from the 19.1 percent average reported two weeks ago.
Notice the omission of the percent positive average from one week ago, which was 20%. A few days later, it went up to 22%. That data wasn't given in the story. I had to look it up, and it's in the screenshot below. No wonder people are skeptical! Incidentally, when I just checked, the current percent positive rate is 17%. Masks didn't work.
Oxford's Centre for Evidence-Based Medicine gives some stern warnings about this sort of bias:
We consider it is unwise to infer causation based on regional geographical observations as several proponents of masks have done. Spikes in cases can easily refute correlations, compliance with masks and other measures is often variable, and confounders cannot be accounted for in such observational research.
And
This abandonment of the scientific modus operandi and lack of foresight has left the field wide open for the play of opinions, radical views and political influence.
And
It would appear that despite two decades of pandemic preparedness, there is considerable uncertainty as to the value of wearing masks.
Here's another overlooked bit of evidence that masks don't work: many Asian countries have been wearing masks for years, especially during outbreaks. Despite heavy mask-wearing, the virus ravaged Wuhan, China. Masks didn't seem to help.
Why masks don't stop the virus
Masks don't work against airborne viruses such as SARS-CoV-2. It can become aerosolized and escape into the air every time you breathe. Obviously, masks allow air to pass through the fabric and around the edges, so they also allow the virus to escape. If you've ever worn a mask and glasses, you've probably had your glasses fog a bit. That's potentially virus-laden air escaping the mask.
You may have heard that the virus attaches itself to respiratory droplets, and that the mask captures those droplets. This is true for large droplets, like the kind you can visibly see when you cough or sneeze. But there are much smaller microscopic water particles that you release every time you exhale. (If you go outside on a cold day and exhale, you can see these condense into a visible vapor.) Many of these either pass through the fabric, or they escape around the edges of the mask. But stopping large droplets isn't going to be much help if you're releasing the virus into the air simply by breathing.
If you have a mask, try this experiment: Put on your mask normally and place a clear glass directly in front of your mouth, being careful not to touch the mask. Exhale forcefully, and see if the glass fogs up. If it does, your mask is letting the virus through.
Now look in the mirror and look for any gaps around the edge of your mask. Hold the glass right next to one of the gaps, and exhale forcefully again. If the glass fogs up... well, you already know what I'm going to say.
Can masks capture at least some of these tiny droplets? Probably. But I've seen no evidence that they capture enough to make a difference. If you have a natural gas leak in your home, can wrapping a towel around the leaking pipe stop some of the gas from escaping? Sure. But is it enough to make a meaningful difference? Probably not.
Scientific studies are sparse and inconclusive
Thus far there have been no large, randomized, controlled, peer-reviewed studies on mask effectiveness against SARS-CoV-2 because it's relatively new. The studies that have been done in 2020 are either non-randomized, not controlled, and not peer reviewed, or they're done using a very small sample size, making the results statistically insignificant. In a meta-analysis of such unscientific studies that specifically looked at SARS-CoV-2, the Lancet said:
Further high-quality research, including randomised trials of the optimum physical distance and the effectiveness of different types of masks in the general population and for health-care workers' protection, is urgently needed.
Incidentally, media outlets have picked up on this meta-analysis and have been touting it as proof that masks work. They obviously missed the part that said the studies The Lancet analyzed were unscientific observational studies.
Prior to 2020, there were many studies done on the effectiveness of masks against the transmission of other viruses. All of these studies have found that when it comes to spreading aerosolized virus particles, there's no statistically significant difference between wearing a mask and not wearing one.
A false sense of security
So, there's no evidence that masks are helping. But are they hurting? Masks make it easier for a person to conceal their illness. Temperature checks are easily defeated by taking analgesics. Throw in a little Benadryl, and you can't tell the difference between someone who's sick and someone who isn't.
For people who are at high risk, masks may present a dangerous false sense of security. Rather than avoiding crowds, an elderly person might attend a large gathering, thinking that they're protected by their own mask or by someone else's. Relying on such an unproven measure as masks is a risky proposition.
Mask are killing small business
Masks are killing small businesses. There are two reasons behind this. First, when people see everyone wearing masks, they conclude that this virus must be really bad, and many will opt to stay home. The psychological weight of seeing masses of people with masks is huge.
Second, small businesses have been put in the awkward situation of being told by their local governments that they must enforce masks for employees, and in some cases, for customers. This introduces more friction into an already tense situation. Business owners want to give the customers a pleasant shopping experience, but they're afraid of being fined or shut down by the authorities if the wrong person complains.
New doesn't mean different
One of the things that rubbed me wrong about the coverage of the coronavirus was the incessant insistence that it was somehow wildly different than anything we've ever seen. "Unprecedented" is a word that suddenly entered the running for most overused words of 2020. But despite what you see in the movies, viruses aren't magic. They can't turn people into zombies, they can't grow wings and fly miles through the air unaided, and they're not indestructible.
Imagine if someone told you that there was a new sort of ransomware that could not only encrypt your data, but could also place a boot on your car and turn your refrigerator into an oven. Would you believe it? Not only would you not believe it, you would probably wonder whether the person telling you this is on drugs. Software isn't magic. Computers operate on a set of rules. So do viruses.
When there's a new or unusual problem, a common mistake is to assume that it requires a new or unusual solution. There's a propensity to assume that the features of other human coronaviruses don't hold true for SARS-CoV-2. But this turns out to be a wrong assumption. SARS-CoV-2 is part of the family of human coronaviruses. Here's what we know about those:
-
Most human coronaviruses—such as OC43, NL63, HKU1, and 229E—cause the common cold, which has a typical incubation period of 1-3 days.
-
SARS-CoV-2 gains entry into cells by attaching to the ACE2 and TMPRSS2 receptors.
-
ACE2 receptors are found in significant numbers on the surface of cells in the lungs, intestines, and arteries.
-
TMPRSS2 receptors are found in the intestinal tract, kidneys, prostate, and pancreas.
-
Both the NL63 coronavirus which causes the common cold and the original SARS coronavirus use the ACE2 receptor also. 229E and the original SARS also use TMPRSS2.
-
The symptoms of the NL63 coronavirus are remarkably similar to SARS-CoV-2—lower respiratory problems like bronchitis and pneumonia.
Almost everyone has been exposed to one of these other coronaviruses, some of which can cause serious illness. They are endemic, and we live with them.
Trying to slow the spread is futile
In April 2020, Swedish physician Johan Giesecke said in a letter published in The Lancet:
Measures to flatten the curve might have an effect, but a lockdown only pushes the severe cases into the future—it will not prevent them.
He turned out to be right. Countries like Sweden that didn't lock down are already well past the peak. Countries that did lock down delayed cases to the present, and we're now experiencing that peak.
It is often quite symptomless and might pass unnoticed, but it also causes severe disease, and even death, in a proportion of the population, and our most important task is not to stop spread, which is all but futile, but to concentrate on giving the unfortunate victims optimal care.
It's time to accept that SARS-CoV-2 is not going away. We're stuck with it. But the good news is that most people will develop immunity to it. And once we reach herd immunity, those few that don't have immunity will be protected.